ACGME Transplant Hepatology Fellowship
The Transplant Hepatology Fellowship Training Program at the University of California is a one year intensive clinical training program designed to comply with ACGME requirements and to provide training that meets ABIM requirements for Board Eligibility for certification in Transplant Hepatology.
Mission Statement and Program Aims
The mission of our fellowship program is to train the future leaders in hepatology and liver transplant through diverse, comprehensive, multidisciplinary clinical experiences in the inpatient and outpatient settings. Our fellows receive outstanding clinical training through direct care of a diverse patient population, as well as a didactic curriculum dedicated to growing their expertise in hepatology. After the completion of the one-year fellowship, fellows have fulfilled all requirements needed to sit for the ABIM Transplant Hepatology exam and work as a UNOS-eligible primary liver transplant physician.






Clinical Program Description
Example Fellow Schedule
| Month | Description |
|---|---|
| JUL | Liver Transplant Unit (LTU) Primary Inpatient Service |
| AUG | Ambulatory Rotation |
| SEP | LTU Inpatient Consult / Ambulatory Rotation |
| OCT | LTU Primary Inpatient Service |
| NOV | Ambulatory Rotation |
| DEC | Ambulatory Rotation |
| Month | Description |
|---|---|
| JAN | Liver Transplant Unit (LTU) Primary Inpatient Service |
| FEB | Ambulatory Rotation |
| MAR | Ambulatory Rotation |
| APR | LTU Primary Inpatient Service |
| MAY | Ambulatory Rotation |
| JUN | LTU Inpatient Consult / Ambulatory Rotation |
UCSF Liver Transplant Program
The UCSF Liver Transplant Program was established in 1998, and nearly 4000 liver transplants have been performed since. We remain one of the largest liver transplant programs in the US, performing 180-200 transplants per year, 20-30 of which are living donor liver transplantations. We evaluate over 400 patients for transplant and add ~200 patients to the waitlist annually. Our pre- and post-transplant outcomes are excellent, despite transplanting extremely ill patients.
Inpatient Experience
The hepatology fellows spend a total of four to six months on inpatient rotations, with a combination of work on the primary service and the consult service.
Primary Inpatient Service Rotation
The UCSF Liver Transplant Unit (LTU) is a multidisciplinary, primary service that cares for liver transplant candidates and recipients, as well as complex liver patients undergoing surgical and/or interventional radiology procedures. The service assumes primary care for patients in the ICU and on the general medical floors. The transplant hepatology fellows play an integral role in the care of patients and education of other trainees who rotate through the service. Our fellows collaborate with the transplant surgical fellows and inpatient advanced practice providers (APPs) to provide care for a complex patient population.
- Team members
- Fellows: transplant hepatology, 2nd year gastroenterology, transplant surgery
- Residents: medicine (2), surgery (1-3)
- APPs
- Social workers
- RN coordinator
- Transplant pharmacist
- RN case managers
- Administrative assistant
- Ancillary services: rehabilitation services, nutrition, speech therapy
- Specific fellow roles on primary service inpatient rotation
- Leadership of the team
- Supervision of interns, APPs, nightfloat residents
- Discussion of liver transplant candidates in weekly selection conference
- Education of trainees (formal and informal)
- Coordination of care
- Procedures for hospitalized patients (e.g., endoscopy, liver biopsy)
- Provide consultative care, split with GI fellow (when no fellow on consult rotation)
Inpatient Consultations
Hepatology consultations are requested by primary services, with consult questions for both common and rare topics within hepatology and liver transplantation. Hepatology fellows provide inpatient consultative service during their consult rotation and/or primary inpatient service rotation. During several months each year, gastroenterology fellows from outside institutions and internal medicine residents assist with performing consultations. Consult requests are shared amongst the hepatology and GI fellows who are rotating on the primary inpatient service.
Ambulatory Rotation
Example Schedule
| Month | Mon | Tues | Weds | Thurs | Fri |
|---|---|---|---|---|---|
|
AUG |
Academic/Admin |
Pre-LT Clinic | Endoscopy | Continuity Clinic | HCC Clinic |
| SEPT | Academic/Admin* | Pre-LT Clinic* | Endoscopy* | Continuity Clinic | HCC Clinic* |
| NOV | Pre-LT Clinic | Pre-LT Clinic | Endoscopy | General Hepatalogy Clinic | Continuity Clinic | IR/OR Obs |
| DEC | Academic/Admin | Pre-LT Clinic | Endoscopy | General Hepatology Clinic | Continuity Clinic | IR/OR Obs |
| FEB | Academic/Admin | Post-LT Clinic | Fibroscan/Endoscopy | Continuity Clinic | HCC |
| MAR | Pre-LT Clinic | HCV | Fibroscan/Endoscopy | General Hepatology Clinic | Continuity Clinic | IR/OR Obs |
| MAY | Selective TBD | Post-LT Clinic | Fibroscan/Endoscopy | Continuity Clinic | IR/OR Obs |
| JUNE | Selective TBD* | Pre-LT Clinic* | Fibroscan/Endoscopy* | Continuity Clinic | HCC* |
Time spent on the ambulatory rotation will expose the hepatology fellows to a broad range of diseases in liver transplant candidates and recipients and patients with common and uncommon liver-related pathology.
Pre-transplant Clinic
10-12 patients are seen in the ambulatory setting each week for a full-day liver transplant evaluation, where they are seen by a hepatologist, transplant surgeon, RN, social worker, and nutritionist. Fellows will perform 1-2 new patient evaluations per pre-transplant clinic session, as well as several patients who are already listed for transplant. The fellows discuss transplant candidates in selection conference on a weekly basis.
Multidisciplinary Hepatocellular Carcinoma (HCC) Clinic
The HCC clinic occurs on a weekly basis, staffed by one of the hepatologists with special expertise in HCC (Drs. Mehta, Zheng, Yao). CTs and MRIs are reviewed in the multidisciplinary tumor board prior to this clinic. Patients are seen by a hepatologist and other providers as indicated (e.g. surgery, interventional radiology, oncology, radiation oncology) in the same clinic session. Fellows participate in this clinic most months of their ambulatory rotations.
General Hepatology Clinic
Most of the hepatologists have a general hepatology clinic in addition to a pre-transplant clinic. A broad range of diseases are seen within these clinics. Additionally, several hepatologists have more specialized expertise in different diseases, such as MASLD (Drs. Hameed, Sarkar, Ha), polycystic liver disease (Dr. Ha), alcohol associated liver disease (Dr. Sherman), women’s health and liver disease (Dr. Sarkar), Asian Liver Health (Drs. Zheng, Yao) and hepatitis C (Dr. Price). The hepatology fellows will work with each of these attending physicians in the respective attending’s clinic and/or in the fellow’s continuity clinic.
Continuity Clinic
Each fellow has their own panel of patients seen weekly throughout the entire year, both during the inpatient and ambulatory rotations. A broad range of patients are followed in this clinic, including liver transplant candidates and patients with hepatocellular carcinoma, MASLD, alcohol associated liver disease, autoimmune hepatitis, viral hepatitis, and many others. The fellows take primary ownership over these patients, with supervision provided by the faculty.
Post-transplant Clinic
Following liver transplantation, patients are cared for by the post-transplant team, which is comprised of APPs and transplant surgeons. Fellows participate in the care of early and late liver transplant recipients, managing surgical and medical problems including immunosuppression, infection prophylaxis, recurrent disease, and/or metabolic syndrome monitoring.
Fibroscan Rotation
An instructional session is provided to the fellows by one of the hepatologists to provide education about the performance and interpretation of Fibroscan. Fellows observe the hepatology techs perform Fibroscan and are then given the opportunity to perform Fibroscan. A repository of Fibroscan images and reports are available to the fellows to assist in their ability to become competent in image interpretation.
Selective Rotation
Fellows are given the opportunity to customize their ambulatory experience during the last quarter of the academic year in order to better prepare them for specific career paths following graduation. The rotations may occur within hepatology/transplant or in other disciplines. Examples of past selective rotations in specialties outside of hepatology include GI oncology (HCC-focused), palliative care, bariatric surgery and addiction medicine.
Telehealth
Telehealth has become an integral part of the care of patients and has been critical in our ability to continue to provide care for patients since the COVID pandemic. Many patients are seen via integrated video visits for both new and established patients in all clinics in which the fellows rotate. Fellows are provided with training around use of telehealth for patient care.
Procedures and Other Clinical Experience
Liver Biopsies
i. The fellows will reach competence in performance and interpretation of liver biopsies
ii. Each fellow will have the opportunity to perform at least 30 percutaneous liver biopsies
iii. The fellows will interpret at least 200 liver biopsies through routine clinical care and a dedicated monthly pathology curriculum in collaboration with the pathology faculty and fellows

Endoscopy
i. Inpatient endoscopies will be performed on an as-needed bases with cases divided between the hepatology and gastroenterology fellows in the inpatient and consult rotations
ii. Fellows on the ambulatory rotation will perform endoscopy weekly with hepatology faculty and can add on additional endoscopy sessions with GI faculty for additional case experience
Procedures Observed
i. Liver transplantation: Fellows will observe at least 2 deceased and one living donor liver transplantation. Fellows will observe one donor procurement.
Didactics and Other Conferences
UCSF is internationally recognized as a leader in research, and the work produced by our group has significantly advanced the fields of hepatology and liver transplantation. The transplant hepatology fellowship offers a rich academic environment, with a wide range of educational and clinical conferences that foster both depth and breadth of training. Under the leadership of Dr. Jennifer Lai, Chief of Hepatology Research, the hepatology research program continues to grow in scope and impact.
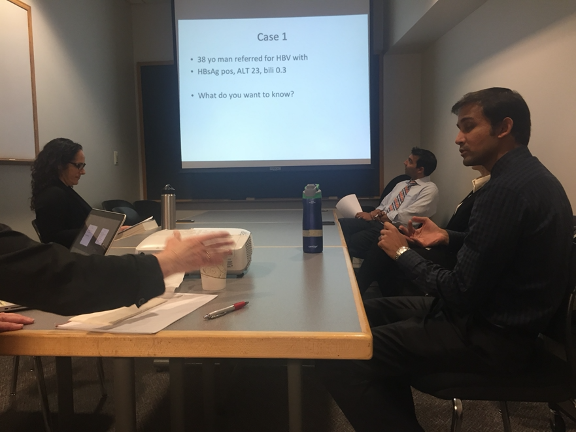
- Fellows participate in a dedicated weekly fellows course, featuring presentations by fellows with faculty discussants, as well as lectures delivered by faculty across hepatology, transplant surgery, and related specialties.
- Monthly journal club provides critical appraisal of two recent high-impact manuscripts.
- Monthly pathology conference offers fellows the opportunity to review and interpret liver histology with expert pathology faculty.
- Fellows participate in twice weekly liver tumor board, where complex imaging studies are reviewed in a truly multidisciplinary setting that includes hepatologists, transplant surgeons, radiologists, interventional radiologists, oncologists, and radiation oncologists.
- Fellows also benefit from access to Gastroenterology Grand Rounds and quality improvement/assurance sessions, ensuring exposure to cutting-edge science, collaborative care models, and system-level thinking.
Conference Schedule
| Morning | Afternoon | |
|---|---|---|
| Mon | 2-2:30pm LTU Intern Teaching | |
| Tue | 2-2:30pm LTU Intern Teaching 4:30-5:30pm HCC Tumor Board |
|
| Wed | 7-8am GI QI/QA (1st Weds.) 8-9am or 8-10am GI Grand Rounds |
12-2pm Transplant Selection Conference 3-3:30pm LTU Intern Teaching 5-6pm Pathology Conference (3rd Weds.) |
| Thu | 4:30-5:30pm HCC Tumor Board | |
| Fri | 7:30-8:30am Transplant Surgery M&M | 2-3pm Tx Hep Fellows Course 3-4pm M&M Conference (3rd Fri.) |
Scholarly Activity

Fellows have the opportunity to engage in scholarly activity, largely during the ambulatory months. Mentorship from hepatology and/or surgical faculty is plentiful. Engagement in quality improvement (QI) activities is encouraged. The goal is for each fellow to complete a project that results in a presentation at a national/international conference and/or manuscript.
Facilities
UCSF is an internationally recognized medical center, and has consistently been ranked within the top 10 medical centers in the US, and is #1 (tied) in California. The UCSF Helen Diller Medical Center and the outpatient clinics are located at the Parnassus Heights campus.
How to Apply
Program Leadership
 Courtney Sherman, MD
Courtney Sherman, MD
Program Director
[email protected]
Svetlana Sogolova
Program Administrator
[email protected]
Nathan Dang
Program Administrator
[email protected]
